Abstract
BackgroundPost-transplant cyclophosphamide (PTCy) effectively prevents graft-versus-host-disease (GVHD) in allogeneic stem cell transplantation (alloSCT) with matched related and matched unrelated donors resulting in low risk of non-relapse mortality (NRM) (<10%). However, PTCy-alloSCT is associated with high relapse rates of approximately 20-30% after 1 year and 30-40% after 2 years (Gooptu et al. Blood 2021, Ruggeri et al. J Hemat Oncol 2018). Prophylactic donor lymphocyte infusion (DLI) may reduce relapse, although it may increase the risk of GVHD.
AimTo provide evidence for reduction of relapse and improvement of survival by combining allogeneic SCT with PTCy and subsequent standardized prophylactic donor lymphocyte infusions (DLI) in a cohort of patients with acute myeloid leukemia (AML) and high risk myelodysplasia (MDS).
Patients and MethodsSixty-five patients with AML (n=50) or high risk MDS (n=15) received myeloablative (n=15) or reduced-intensity (n=50) alloSCT with a matched related (n=8) or 9/10 (n=19) or 10/10 (n=38) matched unrelated donor. Based on modified ELN criteria, 10 AML patients were intermediate risk and 40 poor risk. GVHD prophylaxis consisted of PTCy, mycophenolate until day +30, and tacrolimus tapered from +70 (related or 10/10 unrelated) or day +90 (9/10 unrelated).
All patients were planned to receive DLI at 6 months after transplantation at a dose of 3 x 10^6 CD3+ cells/kg in related and 1.5 x 10^6 CD3+ cells/kg in unrelated alloSCT. In poor risk patients (poor risk AML and high risk MDS) additional low dose DLI (0.3 or 0.15 x 10^6 CD3+ cells/kg in related and unrelated alloSCT, respectively) was planned one month after tacrolimus tapering (i.e. 3-4 months after alloSCT). In poor risk patients with a sensitive molecular or immunophenotypical minimal residual disease (MRD) marker (<0.1%) low dose DLI was not administered but MRD monitored; only in case of MRD positivity at 2 or 4 months additional low dose DLI was given.
ResultsOf the 65 patients, 49 received standard dose DLI at 6 months after alloSCT (75%), either as a first dose at 6 months (40%), or as a second DLI after a low dose DLI at 3-4 months after alloSCT (35%). Reasons for not receiving standard dose DLI were NRM (5%), GVHD (9%), relapse (9%) and donor-related (2%).
Of the 22 poor risk patients with a sensitive MRD marker, 15 received the first DLI at 6 months; 6 received both low dose DLI and 6 month DLI because of MRD positivity at 2 or 4 months after alloSCT; one patient did not receive prophylactic DLI because of systemic relapse at day 105.
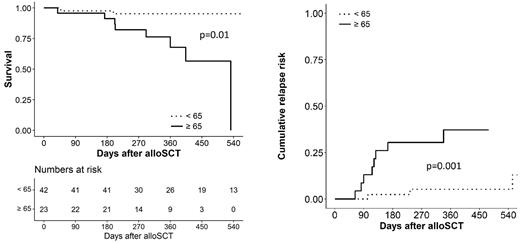
With a median follow up of 400 days (range 183-814), 12 patients developed systemic relapse. Most relapses (67%) occurred very early after transplant (median 110 days, range 63 to 165 days), before low dose DLI could be effectively given. These early relapses occurred significantly more in patients >= 65 years (88%) than <65 years (p=0.01 Fisher's exact).
Overall survival at 1 year was 95% (95% CI 89-100%) in patients <65 (n=42), significantly higher than the 68% (95% CI 49-95%) in patients >=65 (n=23) (p=0.01). Relapse rate at 1 year was 5% (95% CI 1-15%) in patients <65, significantly lower than the 37% (95% CI 25-58%) in patients >=65 (p=0.001). Grade 2-4 acute and chronic GVHD incidence at 1 year was low (6% (95% CI 2-14%) and 11% (2.5-25%), respectively).
Survival at 1 year was similar (p=0.35) in poor risk patients without MRD marker (80%, 95% CI 67-96%), poor risk with MRD marker (95%, 95% CI 87-100%) and intermediate risk (86%, 95% CI 63-100%). For these groups relapse risk was also similar: 18% (95% CI 7-33%), 16% (95% CI 3-36%) and 11% (95% CI 5-41%), respectively.
ConclusionsThis study is the first to demonstrate feasibility of prophylactic DLI after PTCy-alloSCT with a low associated risk of GVHD. The observed low incidence of relapse at 1 year after transplantation (5%) of patients aged <65 years appears to be substantially less than the reported risk without pre-planned DLI (20-30%). Although the value of early DLI administration (around 3-4 months) is still unclear, standard dose DLI administration at 6 months appears feasible in intermediate risk patients and poor risk patients with sensitive MRD markers. Early relapses after alloSCT, at a time point before early DLI could be effective, caused the inferior survival of patients aged >= 65 years. The results of this study can serve as a reference for designing future prophylactic cellular interventions in the PTCy-alloSCT setting.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal